Percutaneous Hydrotomy
Local-Regional Injections for Therapeutic Purposes
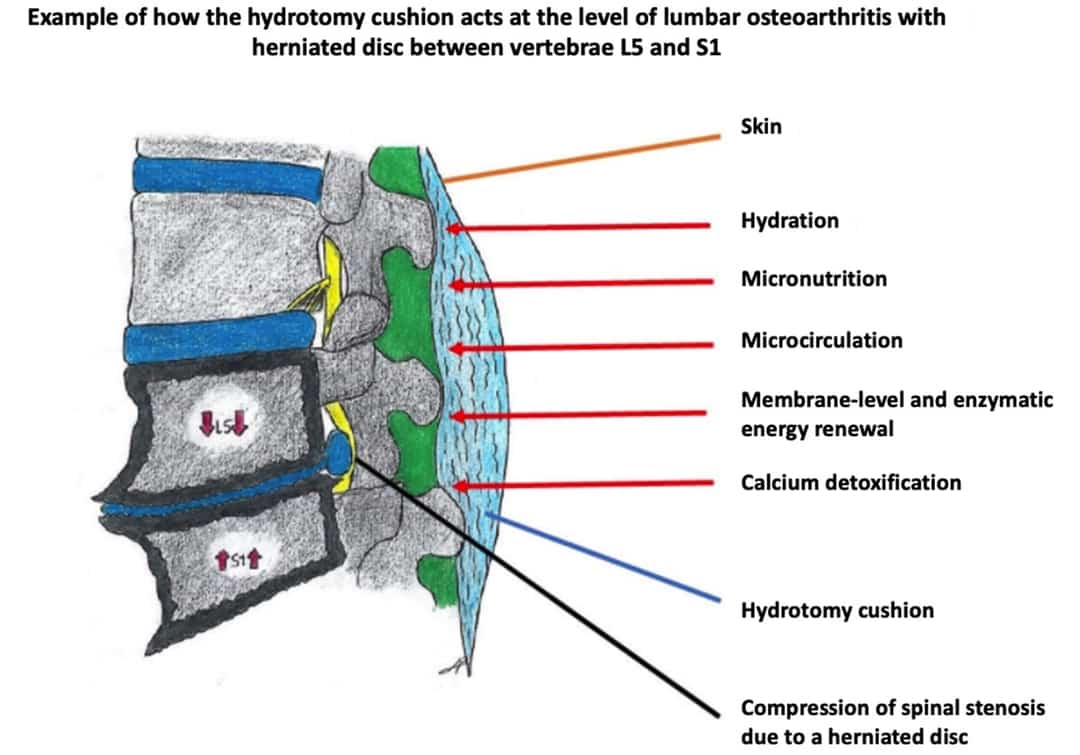
Percutaneous (per·cu·ta·ne·ous) hydrotomy is a medical intervention which consists of subcutaneous or intradermal injection of a physiologic saline solution (NaCl 0.9%). The sterile saline solution is diluted with vitamins, anti-inflammatories, local anesthetics, and trace minerals. Hydrotomy can be used in combination with or prior to other therapeutic medicinal products in line with their scientifically established pharmacodynamic properties. The “hydrotomy cushion” is created by the sterile saline and constitutes a therapeutic delivery vehicle for the other products, leading to localized regional diffusion and absorption helping to treat lesions in a targeted manner. The treatment can be administered discontinuously or continuously in private practice or outpatient settings using the “tumescent” technique.
LOCAL-REGIONAL INJECTIONS FOR THERAPEUTIC PURPOSES
Percutaneous route for:
- Extracellular hydration
- Micronutrition (regenerative medicine)
- Therapeutic delivery vehicle
Percutaneous hydrotomy differentiates technical injection procedures based on the following two criteria:
- The depth of the injection, is usually between 4 and 10 mm, depending on the region targeted: back, neck, shoulder, knees, fingers, etc.
- The injection volume, varies between 5 and 750ml.
Applying the same criteria, the injection varies as follows:
- Single or multiple injections,
- Multipoint subcutaneous infusion can be applied for large areas such as the back.
In addition, during percutaneous hydrotomy low-dose peripheral local anesthetics (xylocaine, procaine) are applied for analgesic purposes during infusion. The hydrotomy cushion is thus targeted to the lesion. This technique has been used for several decades by all practitioners, particularly in general practice when placing stitches or extracting foreign bodies.
Percutaneous Hydrotomy is a melange of hypodermoclysis, mesotherapy, esthetic medicine, and oligo-therapy.
HYPODERMOCLYSIS
Is defined as the subcutaneous injection or infusion of fluids. It is a useful and easy hydration technique. The method is considered safe. Subcutaneous administration of large quantities of physiological solutions. This technique is used to treat large infusion surfaces with drugs and NaCl 0.9% or glucose 5%.
It can be used to supply electrolytes, trace minerals, water-soluble and fat-soluble vitamins, among others.
Therapeutic indications: hydration and nutrition of geriatric and oncology patients, or as part of palliative care.
MESOTHERAPY
First developed by French physician Dr. Michel Pistor, mesotherapy consists of injecting small quantities of drugs “rarely and in the right place” to limit side effects.
Since 1997, Dr Guez has encouraged the development of surface mesotherapy or percutaneous hydrotomy as the mesotherapy of the future, as a means to achieve “true cell washing” or “cellular washout”.
Mesotherapy was recognized by the French Academy of Medicine in 1987, by ANAES (French health authority, now part of HAS) in 2001, and by the French National Order of Physicians in 2002. The technique is taught in medical faculties in Paris, Bordeaux, Lyon and Dijon and all over the world.
Percutaneous hydrotomy uses allopathic conventional medical methods, optimizing their efficacy and safety (depth of injection, products used, large dilutions and small doses), and thanks to their local administration, very clearly reduces the adverse effects of drugs. Percutaneous hydrotomy thus corresponds to a very diluted mesotherapy technique developed over the past decades. It also makes it possible to treat the foundational causes of the disease at the pharmacological level (hydration, micronutrition, detoxification, regeneration, vaccination).
Chronic back pain affect some 16 million adults, and healthcare costs are over 12 billion per year. Back pain is a leading cause of work-loss days, affects all ages and incomes. One in four adults with back pain is in fair to poor physical health and are less active.
Percutaneous Hydrotomy relies on 3 medico-legal principles:
- The validity of local injection, which is a proven technique (listed in the CCAM).
- The use of local pharmacological agents for therapeutic purposes in line with their MA (Vidal).
- The freedom and independence of the doctor’s prescription within the scope of their professional practice and based on their expert knowledge of the patient’s medical history and therapeutic trajectory.
- The patient’s free choice of practitioner.
ADVANTAGES OF PERCUTANOUS HYDROTOMY
Lower back and neck pain are frequently encountered in a medical clinic. The majority of patients presenting with these problems are not surgical problems.
Conventional treatments such as physical therapy, analgesics, anti-inflammatories, spinal injections, etc. do not work or only temporarily. The pain symptoms can be often linked to dehydration of the discs and, very often, pressure on the disc from the upper and lower vertebral plates. Hydration of the intervertebral discs aims to improve vertebral stasis through loco-regional axial re-equilibration across several vertebrae.
Osteoarthritis is an osteo-articular phenomenon reducing the distance between bones. As a consequence, the discs or cartilage is worn down or resorbed, creating a hydro-mechanical problem.
The arthritic process is the result of biological and biochemical modifications at the osteoarticular level. The resulting mechanical inflammation corresponds to the secretion of chemical mediators, or cytokines, and pro-inflammatory substances (prostaglandins, interleukins, TNF alpha, and metalloproteases).
The mediators will modify the loco-regional homeostasis, causing physical-chemical variations (pH, joint osmolarity) in the joint with imbalances in intra- and extra-cellular or intra- and extra-vascular osmolarity, and water imbalances according to the semi-permeable membrane law (Donnan equilibrium). These effects will produce the clinical symptoms of inflammation (pain, redness, heat, swelling).
Whereas anti-inflammatories, which are not without side effects, block a peripheral chemical reaction in pharmacological terms (inhibition of prostaglandin synthesis or anti cox 1 and 2), percutaneous hydrotomy will simply dilute the chemical mediators of inflammation (pro-inflammatory cytokines: interleukins, TNF alpha, metalloproteases in osteoarthritis) while also considerably reducing the side effects by therapeutic cell washing or “washout”.
The opioid analgesics (grade 2) or morphine derivatives (grade 3) frequently used risk leading to habituation with pharmacological dependency in the mid-to-long term. Similarly, anti-epileptics reduce the pain threshold with several side effects. These drugs treat the symptom of pain without treating the hydromechanical cause regulating the plasticity of the osteoarticular ratios (bone, cartilage, discs, nerves, tendons, ligaments, synovial fluid, etc.).Guided injections or spinal surgery can often only treat a single location, e.g. L4-L5. This limitation can lead to recurrence on the same or another disc (L3-L4 or L5-S1) due to vertebral instability. Percutaneous hydrotomy can be used to treat several vertebrae at the same time (L1, L2, L3, L4, L5, S1 (lumbar segment) by ensuring a better distribution of the forces across all the discs involved to re-balance the vertebral stasis. The intervertebral discs work together to ensure suspension of the spine through their strong hydrophilia, the property determining their functional role as shock-absorbers (physical law of disc compliance). Thus, as is often observed, it is possible to treat both early protrusions and herniated discs (start or aggravation of structural degradation to the disc).
After a conventional therapeutic trajectory, to their great satisfaction, many patients were able to discontinue their medication and saw their symptoms disappear thanks to percutaneous hydrotomy. They returned to normal functional activity, including sports activities.
Finally, the very low economic cost of this therapeutic alternative must be underlined as well as its undeniable ecological advantages.
Chronic lumbar pain and neck pain are currently a veritable public health issue with a very significant economic impact.
Based on the body of evidence (studies, publications, communication to expert associations, bibliography, authorized opinions from healthcare professionals, expert analysis of medical records, several hundred testimonies from named patients, etc.), the health authorities should validate this technique, which has been in use for almost 40 years in private medical practice by hundreds of professionals, and is currently being tested with success in anti-pain centers. Percutaneous hydrotomy is the subject of numerous communications, at the national and international levels, and is used on a daily basis by many practitioners trained in the technique. Several scientific studies have been carried out in some University teaching hospitals (e.g. CHU Bordeaux, Lyon, Paris) and private practices.